Neoplasm is an abnormal collection of cells formed by cells that grow continuously on a limited basis, is not coordinated with the surrounding tissue and are not useful for the body.
Cancer is a general term used to describe cellular growth disorder and is a group of diseases and not just a single disease.
Cancer is a general term that includes any malignant growth in any part of the body. This growth was not intended, parasitic and developing at the expense of a man who became the host.
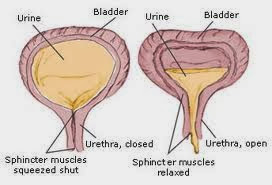
Bladder cancer is a malignant tumor that is found in the bladder (nurse87, 2009)
Symptoms can include:
1. Imbalanced Nutrition: Less Than Body Requirements
related to:
characterized by:
Collaboration:
Rational:
2. Knowledge Deficit about the disease, prognosis and treatment
related to:
characterized by:
Goal:
Read More..
Cancer is a general term used to describe cellular growth disorder and is a group of diseases and not just a single disease.
Cancer is a general term that includes any malignant growth in any part of the body. This growth was not intended, parasitic and developing at the expense of a man who became the host.
Bladder cancer is a malignant tumor that is found in the bladder (nurse87, 2009)
Symptoms can include:
- Hematuria (blood in the urine).
- Burning or pain when urinating.
- Urge to urinate.
- Frequent urination, especially at night and on the next phase of difficult urination.
- Body felt hot and weak.
- Low back pain due to nerve compression.
- Pain on one side because hydronefrosis.
1. Imbalanced Nutrition: Less Than Body Requirements
related to:
- hyper-metabolic-related cancer, the consequences of chemotherapy, radiation, surgery (anorexia, gastric irritation, lack of sense of taste, nausea), emotional distress, fatigue, inability to control pain
characterized by:
- inadequate intake,
- loss of sense of taste,
- loss of appetite,
- weight down to 20% or more below the ideal,
- decreased muscle mass and subcutaneous fat,
- constipation,
- abdominal cramping.
- Showed a stable weight, normal laboratory results and no sign of malnutrition.
- Stated understanding of the need for adequate intake.
- Participate in the management of diet-related illness.
- Monitor food intake every day, whether eating in accordance with the needs of the client.
- Measure weight, triceps size and observed weight loss.
- Assess pale, slow wound healing and parotid gland enlargement.
- Encourage clients to consume high-calorie foods with adequate fluid intake. Instruct too little food to clients.
- Control of environmental factors such as foul odors or noise. Avoid foods that are too sweet, fatty and spicy.
- Create a pleasant dining atmosphere for example, a meal with friends or family.
- Encourage relaxation techniques, visualization, moderate exercise before eating.
- Encourage open communication about anorexia problems experienced by clients.
Collaboration:
- Observe laboratory studies such as total lymphocytes, serum transferrin and albumin.
- Give treatment as indicated.
- Attach a nasogastric tube for enteral feeding, balanced with infusion.
Rational:
- Provide information about nutritional status.
- Provides information about the addition and weight loss.
- Showed very poor nutritional state.
- Calories are energy sources.
- Prevent nausea and vomiting, excessive distension, dyspepsia which causes a decrease in appetite and reduce harmful stimulus which can increase anxiety.
- In order for the client to feel like being at home alone.
- To induce a feeling of wanting to eat / arouse appetite.
- In order to overcome together (with a dietitian, nurse and client).
- To determine / establish the occurrence of nutritional deficiencies as a result of the course of disease, treatment and care of the client.
- Facilitate the intake of food and beverages with maximum results and right as needed.
2. Knowledge Deficit about the disease, prognosis and treatment
related to:
- lack of information,
- misinterpretation,
- cognitive limitations.
characterized by:
- often asked,
- stating the problem,
- statement misconceptions, is not accurate in mengikiuti instruction / prevention of complications.
Goal:
- Can accurately say about diagnosis and treatment at the level of proximity ready.
- Following the procedure well and explain the reasons to follow those procedures.
- Having the initiative of changing lifestyles and participate in treatment.
- In cooperation with the furnisher.
- Review understanding of the client and family about the diagnosis, treatment and consequences.
- Determine the client's perception about cancer and its treatment, tell the client about the experience of other clients who have cancer.
- Give accurate and factual information. Answer the questions specifically, avoid unnecessary information.
- Provide guidance to client / family before following the treatment procedure, the old therapy, complications. Be honest with the client.
- Encourage clients to provide verbal feedback and correct misconceptions about the disease.
- Review client / family about the importance of optimal nutrition status.
- Encourage clients to assess the oral mucous membranes regularly, note the presence of erythema, ulceration.
- Encourage clients to maintain the cleanliness of the skin and hair.
- Avoid duplication and repetition of the client's knowledge.
- Lets do justification to errors as well as errors of perception and conception of understanding.
- Assist the client in understanding the disease process.
- Assist clients and families in making treatment decisions.
- Knowing the extent of understanding the client and client's family about the disease.
- Increasing knowledge of the client and family regarding adequate nutrition.
- Reviewing the development of the processes of healing and signs of infection and problems with oral health can affect the intake of food and beverages.
- Improving the integrity of the skin and head.